
CASE STUDY
Perceptions and Use of Non-Pneumatic Anti-Shock Garments for Management of Postpartum Hemorrhage in Malawi
Prevention, detection, and management of postpartum hemorrhage (PPH)
One of the leading causes of maternal mortality in the world is obstetric hemorrhage in which a woman bleeds heavily, most often immediately after giving birth. The non-pneumatic anti-shock garment (NASG) is a simple, neoprene and Velcro first aid device used to stabilize women who suffer from postpartum hemorrhage and shock.
Ministry of Health and Population (MoH) in Malawi has introduce the NASG in its facilities. Malawi faces patient referrral and transportation issues for expectant mothers causing delays in care. It is an effective tool to reduce PPH related deaths and severe morbidities. NASG use is recommended “in setting where delays in management of PPH are common, particularly where constraints to offer blood products and definitive treatment exist. NASG is an intervention that should be considered as a policy option while the standard conditions for care are being optimized.”
A study was conducted as part of a larger research work led by Advancing Postpartum Hemorrhage Care (APPHC) Partnership on prevention, detection, and management of postpartum hemorrhage (PPH) which continues to be the one of the greatest challenges facing childbearing women in Malawi. As part of the study, the team undertook scoping activities, stakeholder consultations, and a formative assessment between April 2019 and March 2020. The objective was to understand the key implementation barriers, bottle¬necks and opportunities for improved prevention, early detection, and treatment of PPH in Malawi. Specifically, the objective was to seek information on providers’ knowledge, training, perceptions, and use of the NASG; and to identify suitable implementation strategies to improve the use of NASG for management of women with PPH in Malawi.
The mixed method study was conducted in 25 facilities in the districts of Lilongwe, Balaka, Zomba, and Dowa. The surveys included questions on use of NASGs including vignettes that asked providers to describe the actions they would take in the case of PPH, to assess their applied knowledge of PPH management and facility inventories to assess the number of NASGs used at each facility. This was accompanied by inpatient record reviews were also conducted to assess PPH management practices including the use of NASG. Data were also collected via in-depth interviews from providers on introduction of and training related to NASGs, challenges encountered, and how they have been used to reduce morbidity and mortality resulting from PPH in Malawi.
While the MoH published its Integrated Maternal and Neonatal Participants Manual in 2015, protocols on obstetric management for both hospitals and health centers with clear general management for PPH including call for help, explain condition to the woman, apply the anti-shock garment (if available and the provider trained).
Availability of NASGs at facilities
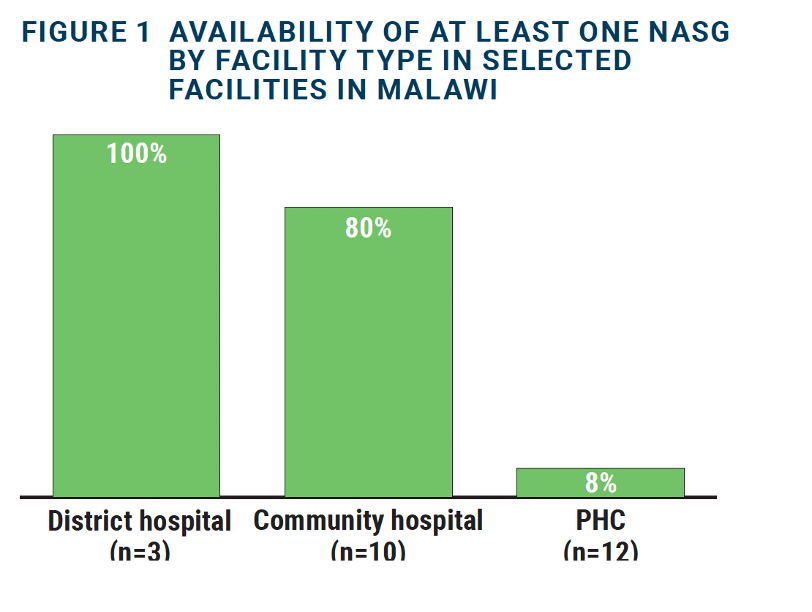
Among the study facilities (n=25), 48 percent had one or more NASGs; 28 percent had one and 20 percent had two. The three district hospitals, 8 community hospitals and one of the primary health centers (PHCs) had at least one NASG available (as shown in the Figure 1 below):
“I have no idea about what NASG is and I have never heard about it and we don’t even have one at this facility.” —IDI, Community midwife, Balaka District
“No, we do not have it. Here we focus on expelling clots, examining, giving oxytocin, and if no improvement we refer them. That’s where we stop.” —IDI, Nurse midwife, Zomba District
“So far here it has not yet been used but we have it. It’s there in our office but eh it’s a long time since I learned that. But it’s what I’ve learned that it’s a good thing.” —IDI, Registered nurse-midwife, Lilongwe District
NASG awareness, training, and experience among providers
Providers also noted a lack of knowledge, training, and experience using the NASG as depicted in the quote below:
The major challenges are lack of resources and knowledge gap. For example, we only have one NASG and again midwives do not know how to apply NASG. —IDI, Nurse midwife, Dowa District
Of the 288 providers interviewed, 13.5 percent reported receiving NASG training in the three months preceding the survey. More providers at district hospitals (19%) were trained in NASG training than community hospitals (15%) or PHCs (8%), as depicted in Figure 2a.
Eleven percent reported using a NASG in the previous three months. Providers who reported they had received training on how to use the NASG reported using it. In addition, providers at district hospitals were most likely to report the use of NASGs (18%) and were most often used in the Dowa district (21%) (Figure 2a and 2b).
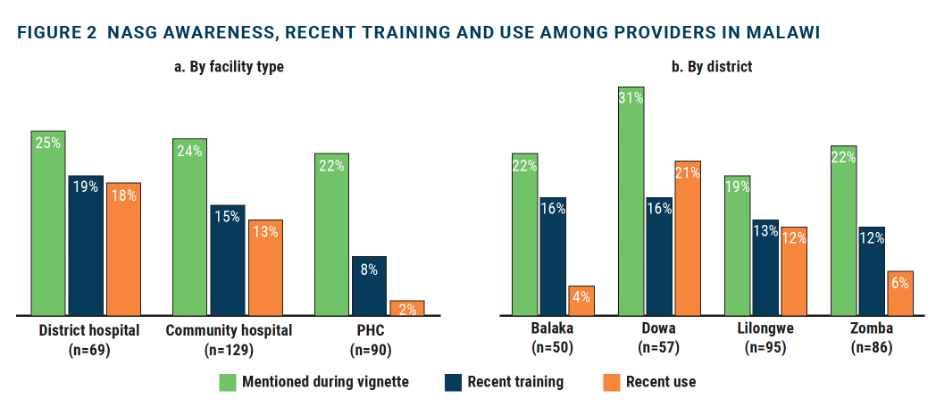
PPH management vignettes and inpatient records of PPH
In response to PPH management vignettes, about a quarter (24%) of providers mentioned the NASG for PPH management. While there was little variation by facility type, providers in Dowa were most likely to mention the NASG (31%), while only 19 percent did so in Lilongwe (Figure 2b). Reviews of 177 women’s inpatient records of PPH highlighted that a NASG was used in only 12% of the instances. District hospitals often used NASG with most documentation in the Balaka district, highlighting the usefulness of NASG in the stabilization and management of PPH as opposed to stabilizing women for transfer.
Below are some quotes on NASG from in-depth interviews highlighting mixed levels of knowledge, training, and experience on how to use the NASG across the different levels of the health system:
“NASG is a very good device and I have seen patients benefiting from it, not necessarily here…but also my previous workplace…. That’s where it was frequently used other than here. For the past two years I have been here NASG was used only once." —IDI, Nurse midwife, Dowa District
“It is good though as of now I don’t have much experience about it. How it is used, and how it controls. Until I know how it works and how they use and how it controls bleeding then I will be very happy.
—IDI, Nurse midwife, Lilongwe District
“I have used the NASG once. We had a patient who developed PPH we did all interventions but the bleeding could not stop the patient started showing signs of shock so like dizziness and postural hypotension so we applied the NASG on the patient.
—IDI, Nurse midwife, Lilongwe District
Barriers to the use of NASG
Across all levels of health facilities, providers noted a lack of training as the barrier to using NASG.
The most basic thing is to train all staff; all midwives should be competent enough to use NASG and be able to know which patient is eligible for NASG, because it’s not every mother who has lost blood can be applied to NASG. —IDI, Nurse midwife, Dowa District
NASGs are an integral part of a continuum of care for PPH. However, they are not designed as a stand-alone intervention, instead, they work to improve outcomes when used as a package of interventions.